HEAD TRAUMA/INJURY:
Introduction.
-Head injuries is the common problem seen at Emergency department.
-Many patient with severe brain injury died before reaching the hospital. 90% of prehospital trauma-related deaths involving brain injuries.
- 75% of patients with brain injuries are categorized as having Minor brain injuries, 15% are moderate and 10% are severe brain injuries.
- 1,700,000 cases of traumatic brain injuries are annual reported in USA, including 52,000 deaths due to traumatic brain injuries.
- survivors from TBI are left with neuropyschological impairment.
Notes
The primary goal of treatment the patients with head injuries is to prevent secondary brain injury.
- Oxygenation and maintenance of blood pressure to provide enough brain perfusion, are very important ways to prevent secondary brain injury.
- To identifying a mass lesion require surgical evacuation is critical and CT scan of the head should performed early as possible.
Risk group
- male age 15-24 years
-young children 6 months to 2 years
- primary school aged student
-elderly
Etiology/causes
-motor vehicle accidents- 50%
-falls- 21%
-violence/assaults- 12%
-sports injuries- 10%
-others-7%
Anatomy review
- cranial anatomy include scalp, skull, meninges, brain, ventricular system and intracranial compartments.
 Scalp
Scalp
- due to several blood supply of the scalp, lacerations can result in a major blood loss, shock, and even death especial in children.

Skull
- injury of the brain occur when the brain move with acceleration and deceleration of the skull because the skull base is regular.
- the anterior fossa contain the frontal lobes, while middle fossa houses the temporal lobe
- the posterior fossa contain cerebellum and lower portion of brain stem.
 Meninges
Meninges
-the meninges cover the brain and consist of three layers; the dura mater, arachnoid mater and Pia mater. Dura matter split to form major venous drainage of the brain.
- superior sagittal sinus drains into the transverse sinus and sigmoid sinuses.
-lacerations of this major sinuses can result into a massive hemorrhage.
-epidural space contain meningeal arteries, overlying skull fracture can lacerate these arteries and cause an epidural hematoma.
-middle meningeal artery located in temporal fossa is commonly injured during head trauma.
-expanding hematoma from arteries in this location can result in rapid deterioration and death. Most epidural hematoma, is an emergency and require evaluation by neurosurgeon as soon as possible.
-veins travel from brain surface to the sinuses may tear during brain injury and lead to the subdural hematoma.
-subarachnoid contain cerebral spinal fluid (CSF). The hemorrhage into this space, is frequently seen during brain contusion or injuries to the major blood vessels at the base of brain.
 Brain
Brain
-major parts are cerebrum, brain stem, and cerebellum. Cerebrum consist of right and left hemispheres
- left hemispheres is a language centers
-frontal lobe control executive function, emotions,motor function and dominant side, control expression of speech.
- the parietal lobe direct sensory function and spatial orientation
- the occipital lobe is responsible for vision and the temporal lobe responsible for regulation of memory function.
- brain stem involve mid-brain, pons, and medulla. Mid brain and pons control state of alertness, while medulla is the vital center for cardiovascular and respiratory system.
- thus the small lesion in the brain stem is associated with severe neurological deficits.
 Ventricular system
Ventricular system
- system filled with cerebral spinal fluid (CSF) and aqueducts within the brain.
- the presences of blood in the CSF, will impair CSF reabsoption and results in increase intracranial pressure
- mass lesion like hematoma can result in a shifting of ventricles that can be easily identified in the CT scan of the brain.
 Intracranial compartments
Intracranial compartments
- tough meningeal partitions separate the brain into regions. The tentorium cerebelli divide the intracranial cavity into the supratentorial and infratentorial compartments.
- midbrain pass through an opening called the tentorial hiatus or notch
- occulomotor nerve run along edge of tentorium and may become compressed against it during temporal lobe herniation.
-compression of these superficial fibers during herniation causes pupillary dilation due to unopposed sympathetic activity, often referred as "blown pupil". Because the parasympathetic fibers that constrict the pupil lie on the surface of the third cranial nerve.
-The part of the brain which usually herniates is the medial part of temporal lobe, known as the
uncus, which may result the compression of corticospinal tract in the brain.
 Notes
Notes
-Ipsilateral pupillary dilation associated with contralateral hemiparesis is the classical sign of uncal herniation.
Blood supply to the brain
- Brain use 20% of total body oxygen and receive 15% of cardiac output. It can also consumer large amount of the glucose and thiamine and it ca not store non of this substance.
- brain receive large amount blood supply from Carotid arteries which supply most of cerebrum and through vertebral arteries which supply cerebellum and brain stem.
 Normal Homeostasis
Normal Homeostasis
- blood flow to the brain should be maintained at constant level. Autoregulation of blood flow to the brain is done in three ways
- pressure- alteration of diameter of blood vessel to maintain SBP of 50 to 160 mm Hg
- Viscosity- occur as a result of changes in blood vessels diameter
- metabolic- brain vasculacture respond quickly to hypoxia which a potent vasodilator and paCO2.
- Brain trauma can impair this autoregulation which in turn, result into hypotension and ischemia which responsible for secondary brain damage.
Physiology
-physiological process involve in head trauma include, intracranial pressure, the Monro-Kellie Doctrine and Cerebral blood flow (CBF).
Intracranial pressure (ICP)
- increased intracranial pressure, can reduce cerebral perfusion and causing ischemia. Normal intracranial pressure is ~ 10mmHg and ICP > 20mmHg are associated with poor outcome.
-As a compensatory mechanism the body produce
Cushing triad which involve:-
- Bradycardia
- hypertension
- irregular breathing
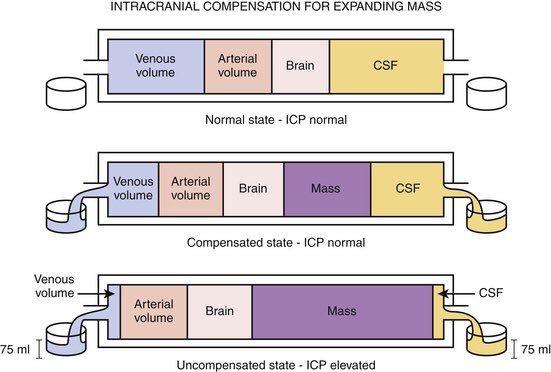
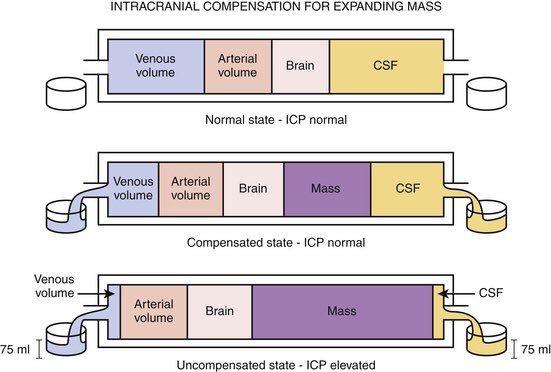
Monro-Kellie Doctrine
- it explain the concept related to ICP, and its stated that; the volume of intracranial contents must remain constant, because the cranium is rigid, non-expansible container.
- at some point/begin, venous blood, CSF, may be squeezed out of the container, providing a degree of pressure buffering ( displacement).
- when the displacement of CSF and intravascular blood has been attained, ICP rapidly begin to raise up.
 Cerebral blood flow (CBF)
Cerebral blood flow (CBF)
- Traumatic brain injury severe enough to cause coma, may results in a marked reduction in CBF during the first hour after injury.
- secondary injury occur due to hypotension, hypoxia, hypercapnia,hypoxemia, and iatrogenic hypocapnia.
- not easy to measure CBF and clinically, cerebral perfusion pressure is used (CPP).
- CPP= ICP-MAP
- MAP= 2/3 DBP + 1/3 SPP
Classification of Head injuries
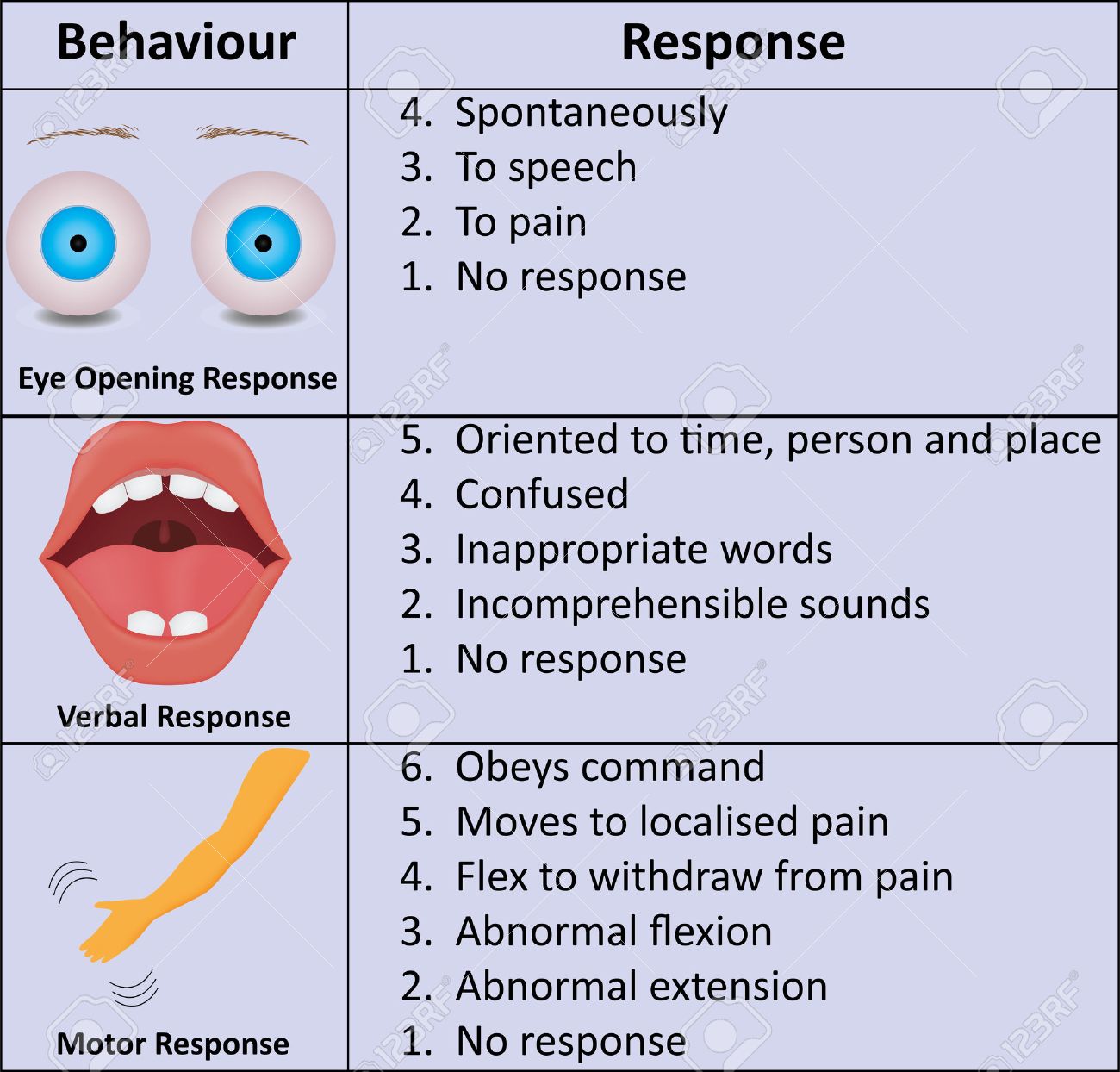
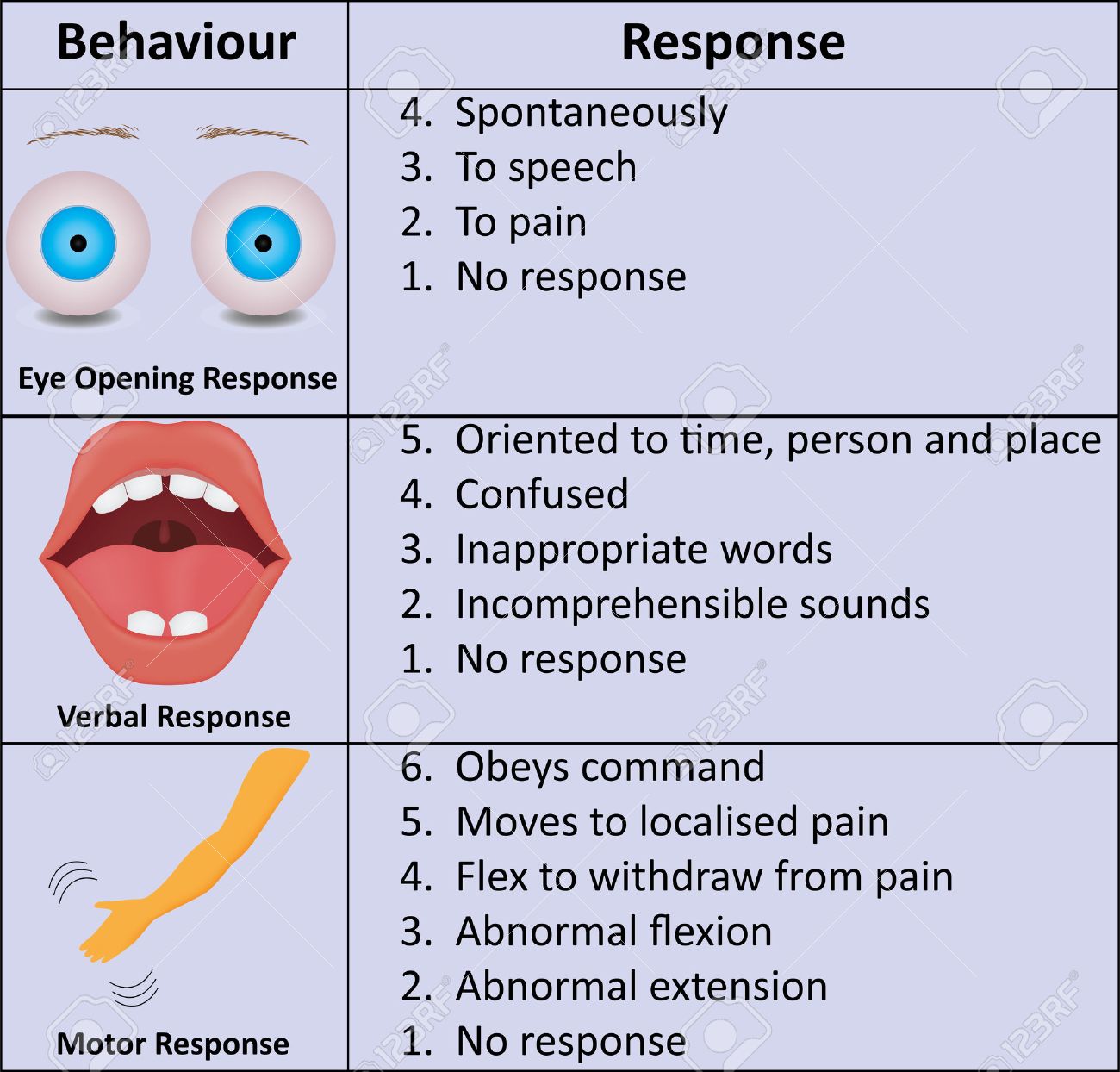
1. according to severity-using Glasgow coma scale
- minor 13 - 15 GCS
- moderate 9 - 12 GCS
- Severe 3- 8 GCS
2. according to morphology
- Skull fractures-vault -linear vs stellate, depressed/nondepressed, open/closed
-
basilar-with/without CSF leak, with/without seventh cranial nerve palsy
- Intracranial lesion- focal- epidural, subdural, intracranial hematoma/lesions
- diffuse- concussion, multiple contusion, hypoxi/ischemic injury and axonal injury.
3. according mechanism of injury
- blunt- closed
- penetrating- open
- Basilar skull fracture require CT scan for diagnosis. The clinical presentation of basilar skull fracture include periorbital ecchymosis ( raccoon eyes), retroauricular ecchymosis ( Battle sign).
- CSF leakage from the nose or ears and seventh and eight cranial nerves dysfuction may other signs for basilar skull fracture.
- CSF suspected tests include blood clotting delayed, halo sign ( Ring sign), does not crush on drying and positive to dextrostick.
Note
- in basilar skull fracture, do not pack ears, not sucking fluid, not instrument the nose, allow drain, and gives antibiotics for prophylactic.
- open skull fracture should be managed like evisceration and protecting exposed tissue with moist, clean dressing.
Intracranial lesions
1. Epidural hematoma
- blood collect between the skull and dura, usually caused by tear of middle meningeal artery.
- it associated with increased ICP, unconsciousness followed by lucid interval, headache, nausea vomiting, hemiparesis, hemiplegia, unequal pupils( dilated on side of clot) and cushing triad.
 Subdural hematoma
Subdural hematoma
- more common types and it occurs between dura mater and arachnoid mater.
- usually develop following a tear of bridging veins between cortex and dura. This type of hematoma is also associated with increase ICP, but usually of slow onset. These symptoms are of same as epidural hematoma.
Intracranial hematoma
- occur following brain laceration and bleeding into brain develop. Associated with increased ICP, neuro deficit ( depending on the part of brain affected).
Assessment of brain injuries
1.Glasgow Coma Scale (GCS)
-severity of brain injury is scored using GCS and it was pointed out in the area classification of brain injuries.
2. AVPU scale
A= Alert
V= Respond to verbal stimuli
P= Respond to pain stimuli
U= Unresponsive
3. Respiratory pattern
- cheyne stoke due to diffuse injury to cerebral hemispheres
- central neurological hyperventilation due to mid-brain injury
- apneustic due to pons injury
4. eyes- unequal pupil dilation- pointed out before in this presentation
5. vital signs- cushing triad ( Hypertension, bradycardia and irregular respiratory patterns) due raise in ICP.
- Part of management involve ABCDs
A. Airway
-open, consider cervical spine injury
-jaw thrust with cervical spine control, clear airway, intubate the patient as needed, but avoid nasal intubation.
- spinal motion restriction
B. Breathing
- give 100% of oxygen, hyperventilate at 20 and 24 breaths per minute if GCS is less than 8, presences of neurological deterioration and evidence herniation.
- hyperventilation will decreased paCO2, vasoconstrication and decreased ICP, but it may increase risk of decrease cerebral blood flow, decrease perfusion of tissue, and increase edema.
C. Circulation
- the role is to maintain adequate BP and brain perfusion by use IV fluids
- gives RL/NS if BP is normal or elevated
- gives RL/NS bolus titrated to BP ~ 90 mm Hg in case decreased blood pressure.
D. Drugs
- dexamethasone- decreases cerebral edema but effect delayed
- mannitol - decrease cerebral edema but it may cause hypovolemia or worsen intracranial hemorrhage.
- furosemide- decrease cerebral edema, but may cause hypovolaemia
- diazepam- given in patient with seizures, but it may mask level of consciousness, depressed respiration and worsen hypotension.
- glucose- gives hypoglycemic patient
Investigations
- CT scan of brain
- skull X-ray
- MRI
- Cerebral angiography in case of vascular injury
- ventriculography
Basic neurosurgical procedures
- external ventricular Drainage- ventriculostomy
- exploratory or woodpeker surgery - exploratory burr holes
- Craniotomy/ craniectomy
Thanks
MWANDA MD!